Vascular
 A number of progressive metabolic diseases, especially diabetes, accelerate
arthrosclerosis leading to an increased rate of myocardial infarction,
cerebrovascular stroke, and other complications of narrowed or occluded
arteries. Equally prevalent is the impairment of peripheral circulation
which deprives organs and limbs of oxygen leading to tissue ischemia and
eventual tissue death. As the condition progresses, the lack of oxygen leads
to pain upon exertion and, at the advanced stage, gangrene. Complications
from these conditions are the leading cause of limb amputation.
A number of progressive metabolic diseases, especially diabetes, accelerate
arthrosclerosis leading to an increased rate of myocardial infarction,
cerebrovascular stroke, and other complications of narrowed or occluded
arteries. Equally prevalent is the impairment of peripheral circulation
which deprives organs and limbs of oxygen leading to tissue ischemia and
eventual tissue death. As the condition progresses, the lack of oxygen leads
to pain upon exertion and, at the advanced stage, gangrene. Complications
from these conditions are the leading cause of limb amputation.
Stem cells promote formation of new endothelial tissue, the building blocks for arteries, which can then vascularize the ischemic tissue and reduce amputation rates. Compelling data exists for two indications:
-
Peripheral arterial disease
-
Thromboangiitis obliterans (Buerger’s disease)
Peripheral Arterial Disease (PAD)
PAD is a frequent complication of diabetes. Like most atherosclerotic diseases, it is a progressive condition eventually resulting in chronic pain even at rest, the point at which it is considered critical limb ischemia; a major limb amputation normally follows within six months. The root cause of this condition is narrowing of the arteries at the far extremities, such as the feet and toes.
 The convention
surgical treatment for PAD is a vascular intervention designed
to improve microvascular circulation through an arterial by-pass. An
arterial by-pass works by creating a secondary path from the femoral artery
above the knee to the popliteal artery below the knee, thus improving
circulation to the extremity. This is a major surgery requiring
general anesthesia and depending on the condition of the patient's
vasculature, it may only be a stop-gap measure as the vessels can reocclude.
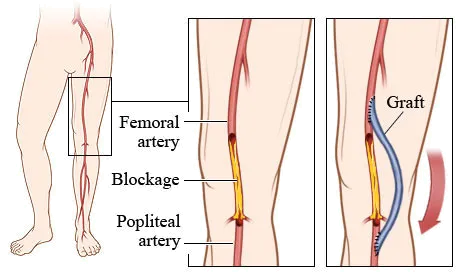
The convention
surgical treatment for PAD is a vascular intervention designed
to improve microvascular circulation through an arterial by-pass. An
arterial by-pass works by creating a secondary path from the femoral artery
above the knee to the popliteal artery below the knee, thus improving
circulation to the extremity. This is a major surgery requiring
general anesthesia and depending on the condition of the patient's
vasculature, it may only be a stop-gap measure as the vessels can reocclude.
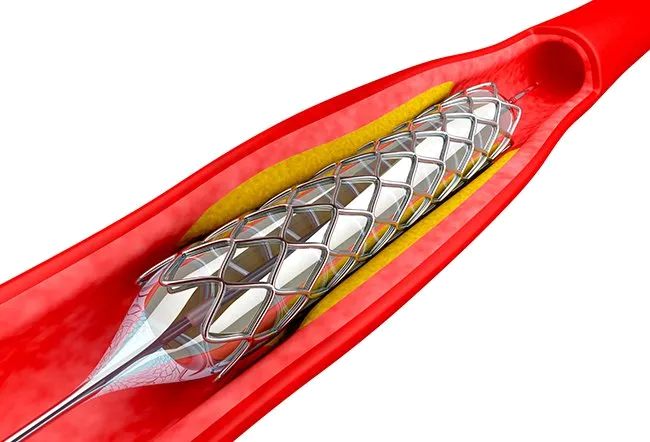 An alternative to by-pass surgery is an intravascular stent. Stents
are small wire mesh cages that are inserted directly into the partially
blocked vessels using a balloon catheter. Once the stent is positioned
properly, the balloon is temporarily inflated, the wire mesh deforms to open
the vessel, after which the balloon is deflated and withdrawn leaving the
stent behind.
An alternative to by-pass surgery is an intravascular stent. Stents
are small wire mesh cages that are inserted directly into the partially
blocked vessels using a balloon catheter. Once the stent is positioned
properly, the balloon is temporarily inflated, the wire mesh deforms to open
the vessel, after which the balloon is deflated and withdrawn leaving the
stent behind.
Stent placement can frequently be done without general anesthesia and it requires only a small incision to introduce and remove the balloon catheter. Ultimately it suffers from the same drawback as by-pass surgery in that the stent itself can become blocked and the overall condition of the patient's vasculature is not improved.
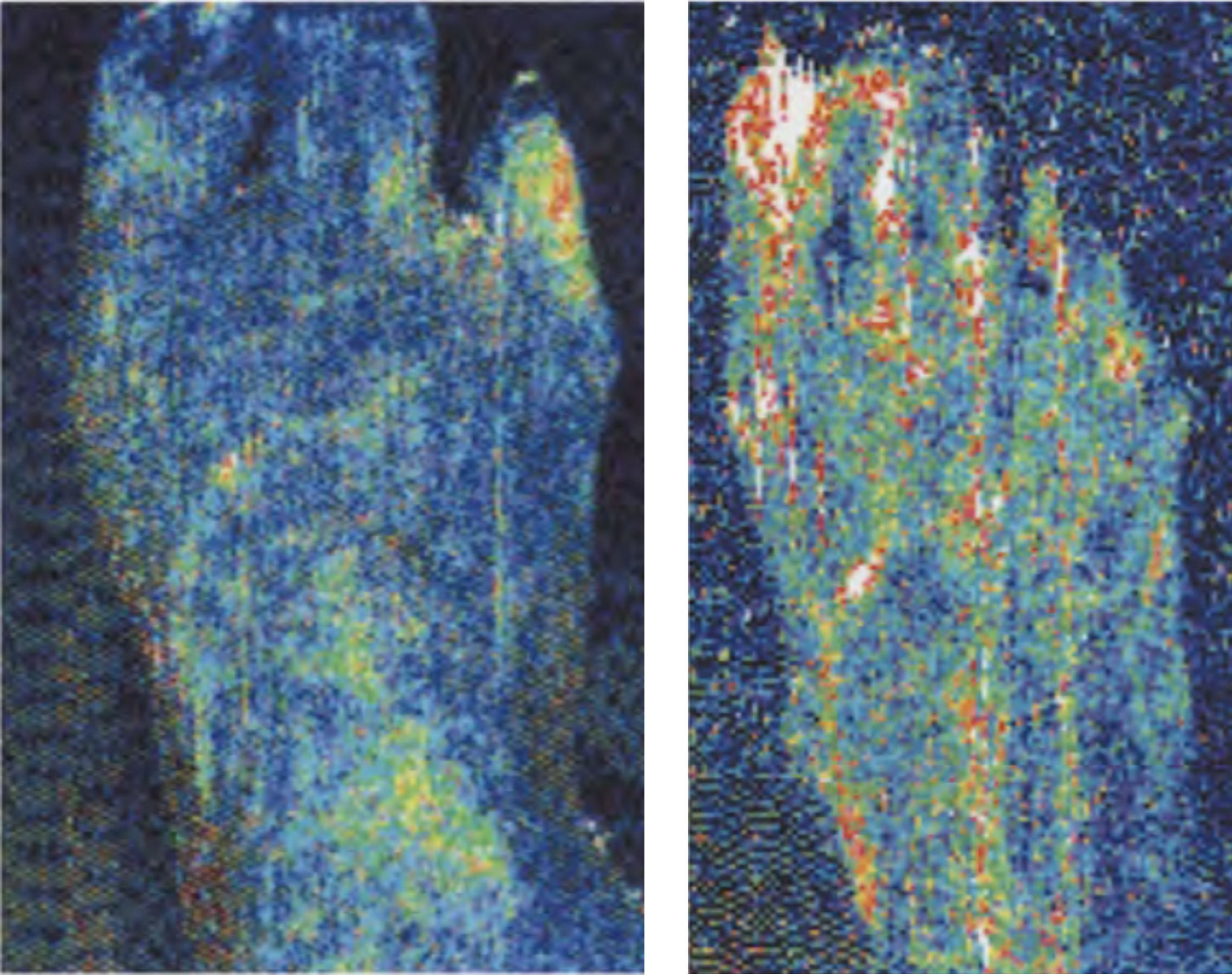
The cellular therapy alternative is to create new collateral circulation. A bone marrow aspirate is processed and the cells are injected directly into the affected area where the stem cells create new arteries. The images below show thermography images before and after treatment with cells (left side image show lack of circulation, right side image shows new vessel formation and improved perfusion)1. Because this therapy is actually creating new collateral blood vessels, it is more robust than by-pass surgery or stent as the new vessels are themselves free of atherosclerotic plaque.
Thromboangiitis Obliterans
Buerger’s disease, also called thromboangiitis obliternas, results from chronic inflammation of arteries and veins. The most frequent cause is smoking or use of chewing tobacco, and is seen most commonly in males and older adults. While the exact mechanism of damage is slightly different from that of peripheral arterial disease, the end result is the same as the blood vessels become increasingly occluded. Treatment with stem cells, in a manner similar to that described above for PAD, has proven effective in reducing pain and avoiding amputation.



