


 Cascia
Cascia
 Immunoregenerative Peptides
Immunoregenerative PeptidesOligodeoxynucleotides are small fragments of protein that enter the cell by exocytosis and are designed to prevent or modulate the translation of specific genes, thus providing a means of altering cellular functions that have not been modifiable by traditional drugs. A growing number of peptide drugs have been approved by the FDA and other regulatory agencies, and many more are in development or are undergoing clinical studies. Virtually all peptides share the CpG motif, a segment with a cytosine triphosphate nucleotide linked to a guanine triphosphate nucleotide by a phosphodiester. These peptides are recognized as PAMPs (pathogen-associated molecular patterns) by the immune system, which triggers an appropriate response to fight the pathogen. In addition to their use in treating disease, because these peptides stimulate an immune response they are often used as an adjuvant to improve the potency of vaccines.
An alternative class of peptides, ones that do not rely on the CpG motif, has been discovered that creates both immunological and regenerative effects. Like CpG peptides, these are recognized by cells of the immune system, but not as pathogens. The behavior of these peptides is not fully understood, but it is believed that they function as DAMPs (damage-associated molecular patterns), which are recognized by the innate immune system. DAMPs are released when cells are damaged, either by disease or trauma, and they trigger an noninfectious inflammatory cascade designed to mitigate further injury by expelling invaders from the affected tissue and initiating the tissue repair process. DAMPs can be released from the nucleus, cytosol, mitochondria, endoplasmic reticulum, granulocytes, plasma membrane, or the extracellular matrix, and once released they interaction with one of numerous pattern recognition receptors.
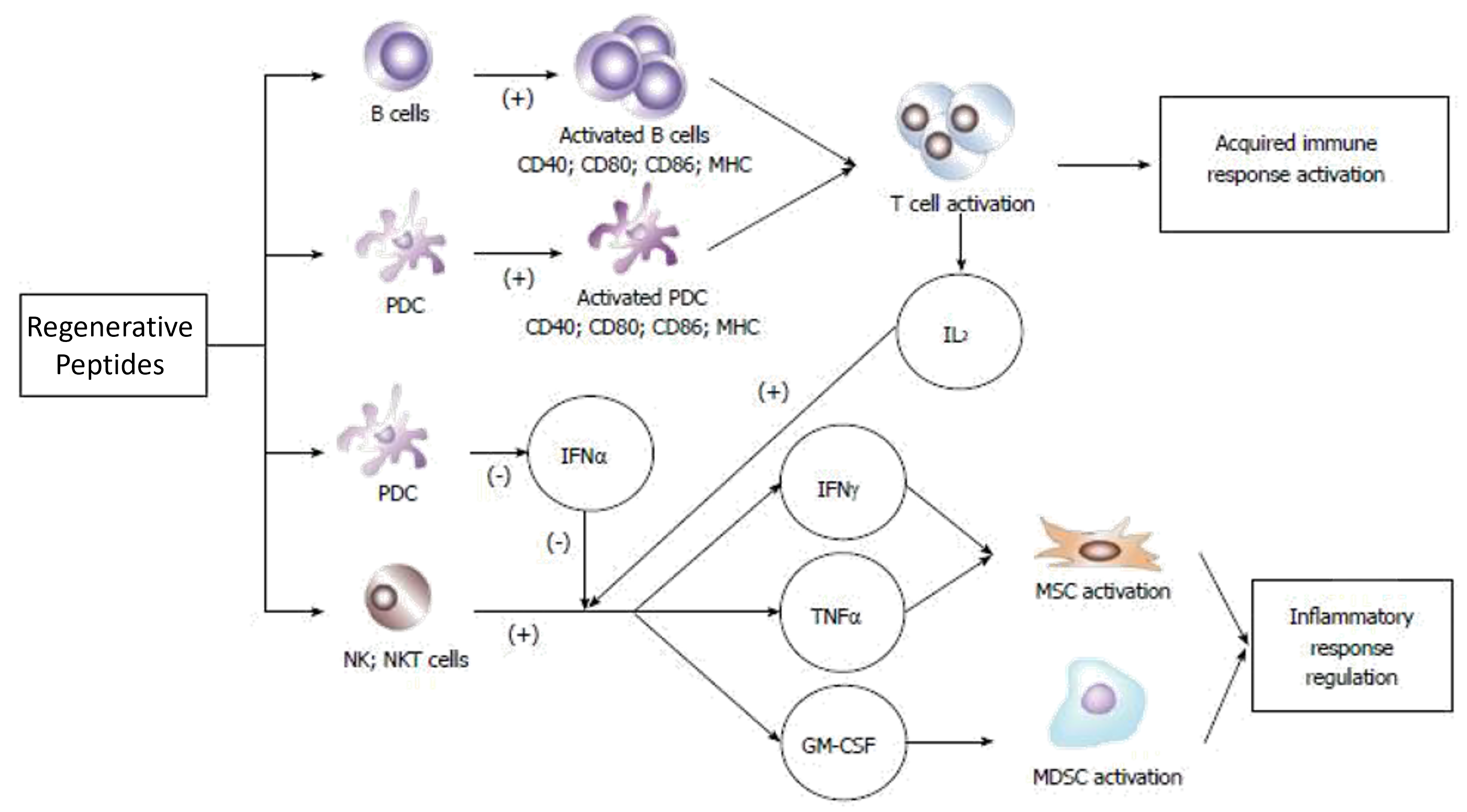
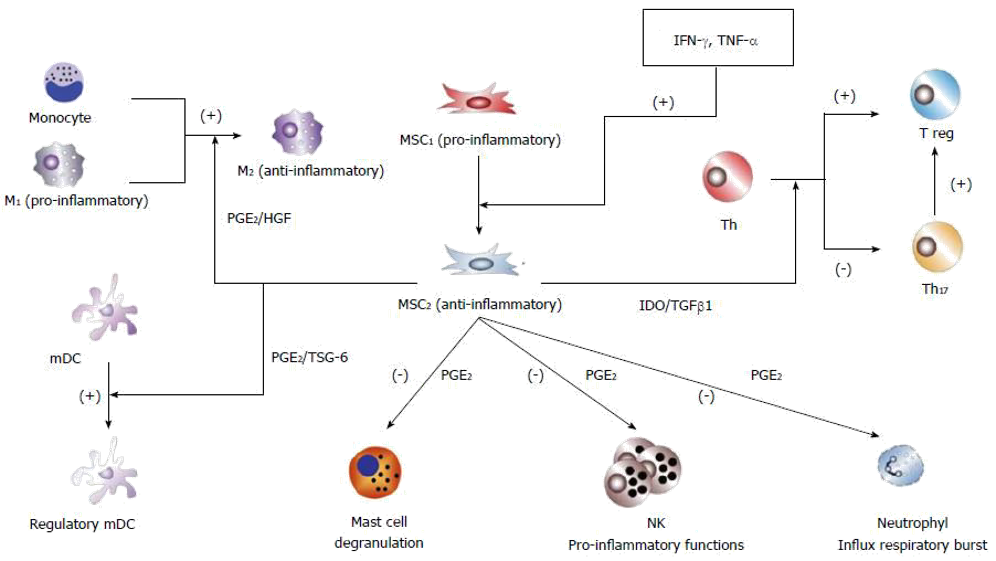
These non-CpG peptides have the ability both to stimulate an immune response to fight infections, and to activate and initiate replication of mesenchymal stem cells (MSC). A principal function of MSCs is to expand in number and to differentiate into the various tissues that originate from the mesenchyme, but stem cells are also known to down-regulate the inflammatory response following injury by repolarizing macrophages from their pro-inflammatory M1 phenotype to the anti-inflammatory M2 phenotype. When inflammation is attenuated, other symptoms associated with the inflammatory cascade, such as swelling and pain, are likewise reduced.
.
The dual-ability to modulate the immune response while at the same time initiating tissue repair can be applied to many different disease and injury states. The feasibility of using these peptide therapeutics have been demonstrated in a variety of applications in animal experiments, and on a limited number of human subjects. These include:
Inhibition of liver fibrogenesis progression and reversal of established fibrosis
Diabetes, both Types I and II, accomplished by beta islet regeneration
Sepsis, and potentially other systemic immune
conditions such as lupus erythematous
Multiple sclerosis and other demyelinating
diseases