



 Cascia
Cascia

Stem cell therapy has show promise in liver regeneration applications. While the liver, unlike other ograns, has the ability to regenerate naturally, when disease is present its natural mechanisms may not be sufficient. There are two indications in particular where stem cells may be extremely beneficial:
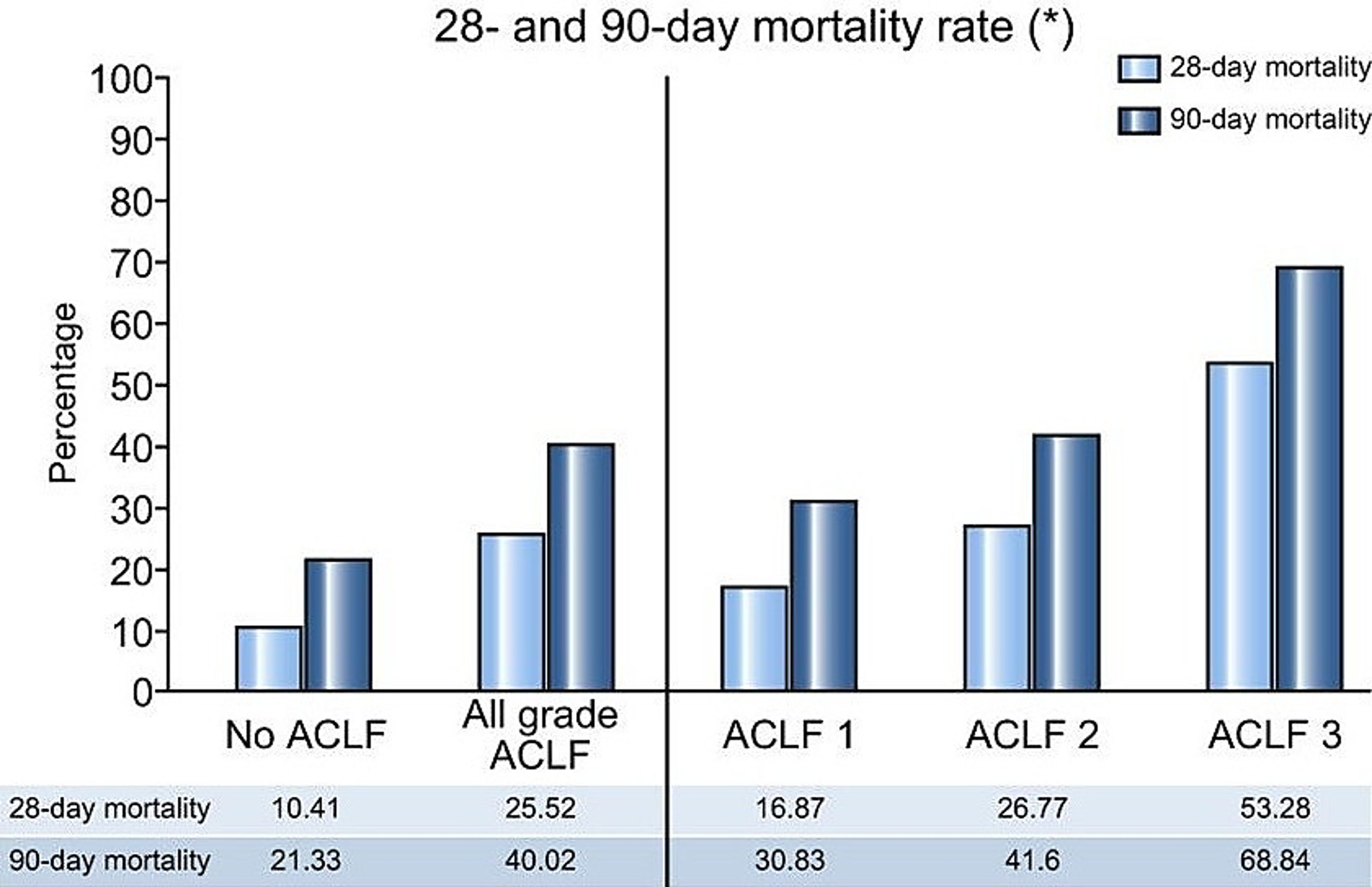
Acute liver failure, also known as fulminant hepatic failure, is a rare and serious condition where the liver suddenly stops working. The underlying cause of acute failure varies but the two most common auses are toxicity, such as acetaminophen overdose or exposure to environmental toxins such as heavy metals, and progression of chronic liver disease such as hepatitis. The term acute-on-chronic liver failure (ACLF) has been used to define a syndrome in patients with acutely decompensated cirrhosis and association with an intense systemic inflammatory response. The most common precipitating conditions are infections, alcoholic hepatitis, and other organ failures.The 28‑day mortality rate for ACLF is estimated to be 26% overall, with higher rates for the more severe forms
Liver failure, regardless of the cause, is a severe medical
condition requiring immediate treatment.
The liver interacts with other organs and failure is often accompanied by
severely reduced kidney function, encephalopathy (swelling of the brain due to
accumulation of toxins that affect the brain, such as ammonia), and coagulation
failure.
 There is a rapidly growing incidence of MAFLD (metabolic
dysfunction-associated fatty liver disease) and its associated condition MASH
(metabolic dysfunction-associated steatohepatitis).
Fatty liver disease is the buildup of small fat particles in the liver, largely
as a result of poor dietary habits, lack of exercise and other lifestyle issues.
There is a rapidly growing incidence of MAFLD (metabolic
dysfunction-associated fatty liver disease) and its associated condition MASH
(metabolic dysfunction-associated steatohepatitis).
Fatty liver disease is the buildup of small fat particles in the liver, largely
as a result of poor dietary habits, lack of exercise and other lifestyle issues.
The precise incidence of fatty liver disease is difficult
to establish because there are no obvious symptoms until the condition
progresses. A definitive diagnosis can only be made with a histological
analysis of their liver tissue following a biopsy, or magnetic resonance imaging
of their abdomen. Neither are routine diagnostic procedures performed in
the absence of other symptoms.
As the chart at left shows, there is clearly a genetic
component as well since more than half of adults of Hispanic ethnicity have
fatty liver disease compared with about a third of African Americans.
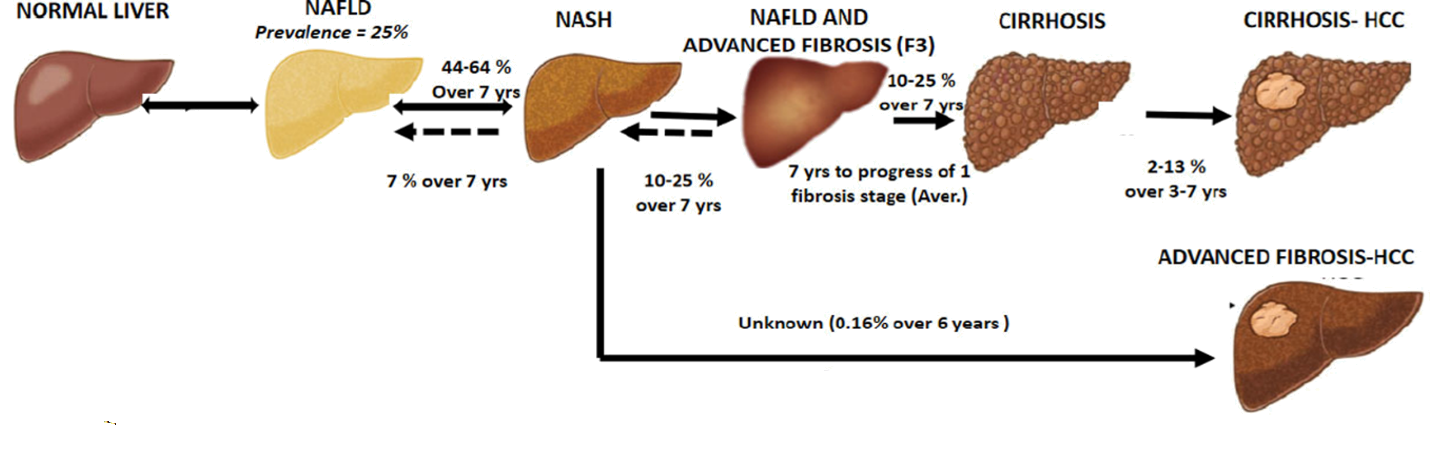
MAFLD is often a progressive disease, with about half of
the patients progressing to MASH over a seven-year period. MASH is quite
similar except that enough liver tissue has become scarred at that point that a
physician can feel the difference in elasticity when making a manual examination
of the abdomen, and there may be changes in liver enzyme levels.
If MASH is not treated, an estimated 1 in 4 patients will progress to more serious fibrosis, cirrhosis, or hepatocellular carcinoma.
The liver exhibits a tremendous ability to regenerate
itself to an extent not found elsewhere in the human body, but when a
progressive disease becomes too advanced this capability is not sufficient to
maintain liver health. A liver
transplant is often the recommended solution, but there is a chronic shortage of
transplant organs with an estimated 1,400 patients eligible for transplant
dieing before an organ becomes available, and there are additional patients who
are not eligible due to age, overall physical condition, or presence of
disqualifying factor such as active infectious disease.
d
chemistry values, especially albumin. Several investigators have administered
mesenchymal stem cells to patients with acute liver failure with reports of
promising results, albeit on a limited number of patients, with decreased MELD
scores and improved blood chemistry. Stem cell treatments hold the promise to
obviate the need for a liver transplant in some cases, and to increase the
amount of time the patient can survive while waiting for a transplant organ to
become available. The MELD score is frequently used by transplant teams to
estimate the risk of death without a transplant, so a decreased MELD score is an
indicator of increased survival.